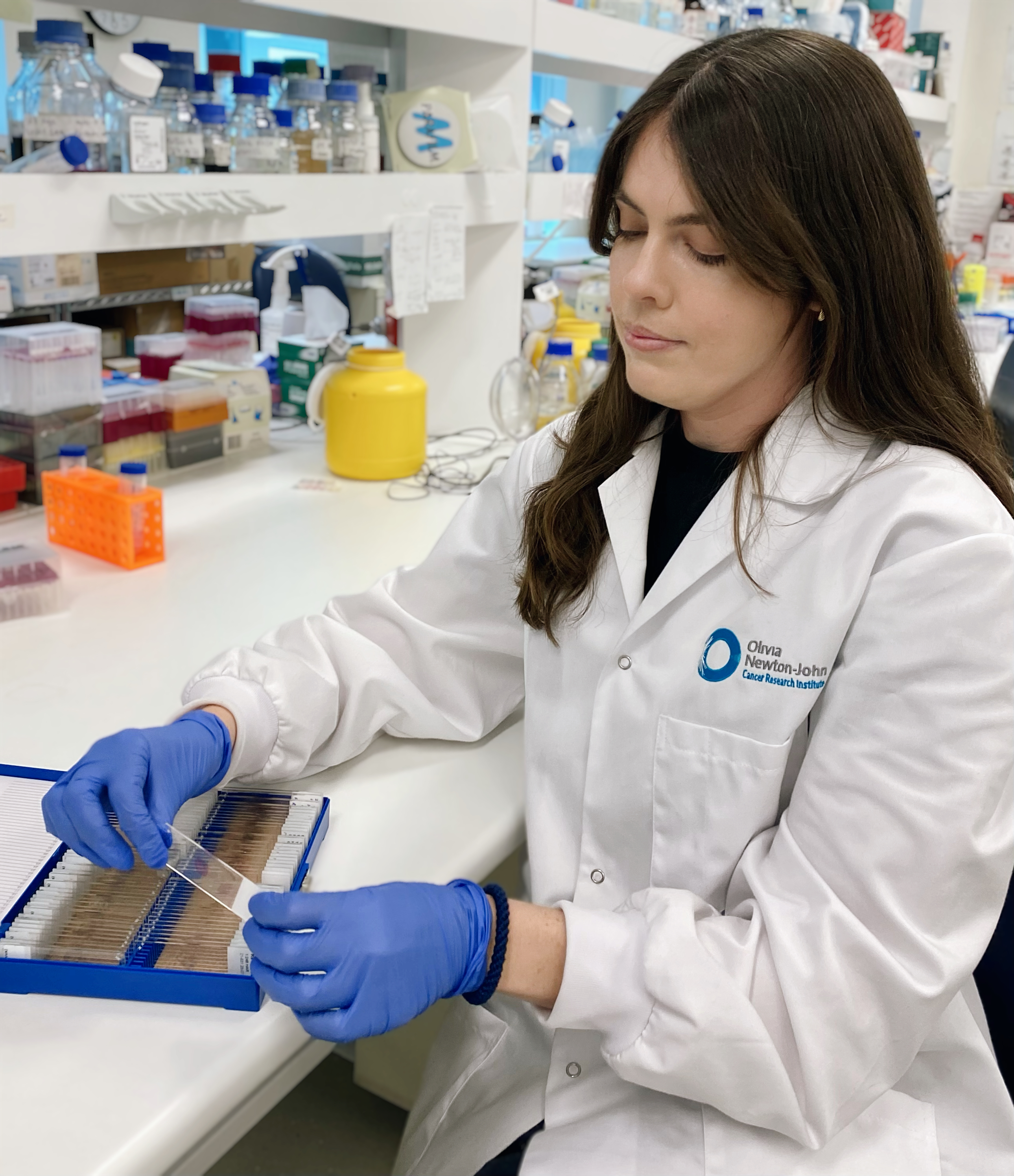
Bringing hope to families: Meet the researchers working to cure childhood cancer
By Emily Usher | 12 July 2024
An estimated 400,000 families around the world are devastated by a childhood cancer diagnosis each year. Today, we highlight 4 brilliant researchers who are committed to changing the outlook for children today and in the future.

Every year, more than 1,000 Australian children are diagnosed with cancer, with nearly half receiving this life-altering diagnosis before they turn 5 years old. These young lives, just beginning, are suddenly overshadowed by hospital visits, gruelling treatments, and long-term health challenges.
Childhood should be a time of joy and exploration, not pain and uncertainty. The harsh reality of cancer treatments disrupts their development and leaves lasting impacts. However, there is hope. Through dedicated research, we can transform these children's futures, developing treatments that are more effective and less harmful.
This is why Cure Cancer is committed to funding the brightest scientists focused on finding a cure for childhood cancers. Their groundbreaking work holds the promise of a future where no child has to endure the suffering caused by cancer. Meet 4 of these inspiring researchers and learn how their efforts are making a difference.
Dr Ben Wylie – Childhood Sarcoma Researcher
Project: Developing novel immunotherapies to prevent the recurrence of sarcoma after cancer removal surgery
Telethon Kids Institute, University of WA

Every year, more than 75 children under the age of 15 in Australia are diagnosed with sarcoma. Tragically, 2 out of 5 of these children will lose their lives to this disease.
Sarcoma is a tough and aggressive type of cancer that affects the bones and soft tissues. It’s rare in adults but hits kids and teenagers much harder, making up 20% of cancer cases in people under 20.
Children with sarcoma face a high risk of the cancer coming back, which is a major reason for cancer-related deaths. When sarcoma returns, kids often need more chemotherapy or radiotherapy, which can have serious long-term side effects and may not work well.
The main treatment for sarcoma is usually surgery to remove the tumour. However, if any part of the tumour is left behind, the cancer can come back. When this happens, the follow-up treatments are less effective and can cause severe, lifelong problems.
“Most new cancer treatments are developed for adults and then adapted for childhood cancers. But children are not just little adults. Support for childhood cancer research is vital, to provide better treatments for childhood cancers like sarcoma, and better outcomes for children and their families."
- Dr Ben Wylie
Through conversations with cancer surgeons, Dr Ben Wylie understood that recurrence after surgery was a big problem for sarcoma patients. The surgeons knew that sometimes they couldn’t remove all the cancer and, if even microscopic cancer cells were left behind, the cancer could potentially come back. They needed a way to eliminate those cancer cells to improve the outcome for patients’ post-surgery.
Dr Ben and his team engineered the gel so it could be loaded with anti-cancer drugs and delivered into the surgical area, during cancer removal surgery. The gel is made from natural materials found in the body, and this allows the body to break it down over time. As the gel is broken down, it slowly releases the drugs contained inside around the surgical area. These drugs activate the patient’s immune system to seek and destroy any remaining cancer cells.
This work has the potential to produce an entirely new way for surgeons to deliver therapy for patients who are already having surgery to remove their cancer, one that may help to reduce the rate at which cancers, like sarcoma, recur after surgery. This could lead to oncologists needing to rely less on follow-up chemotherapy and radiotherapy and help patients achieve better, long-lasting outcomes after their treatment.
A/Prof Orazio Vittorio – Childhood Brain Cancer Researcher
Project: Blocking copper uptake in glioblastoma tumours to boost their immune response
The University of NSW (UNSW Sydney)

Brain tumours are the leading cause of cancer deaths in children and adults under 40. Neuroblastoma and glioblastoma are particularly deadly for children, with very low survival rates. Neuroblastoma causes 15% of childhood cancer deaths, and only 5% of children with glioblastoma survive beyond five years. Those who survive often face lifelong side effects from treatment.
“Childhood cancer is considered rare, and so research is underfunded by both the government and pharma companies. But if we consider the impact that cancer has on children with their entire lives in front of them, and the impact on their families, childhood cancer patients cannot be considered less worthy of support."
- A/Prof Orazio Vittorio
Neuroblastoma and glioblastoma tumours have high levels of copper, which helps them grow. Cure Cancer-funded researcher A/Prof Orazio Vittorio and his team have developed a new compound that targets these high copper levels, killing cancer cells while being less toxic than chemotherapy. They discovered that by removing copper from the blood, they can make these cancers more vulnerable to the immune system.
This breakthrough could change how we treat these cancers, potentially eliminating the need for chemotherapy and reducing long-term side effects. Orazio is now preparing for clinical trials to test this new treatment, aiming to improve survival rates and quality of life for patients.
Dr Laurence Cheung – Childhood Leukaemia Researcher
Project: Understanding leukaemia and restoring bone marrow in children with leukaemia
Telethon Kids Institute and Curtin University

Acute lymphoblastic leukaemia, or ALL, is the most common type of blood cancer in children. Thanks to better treatments over the past sixty years, the cure rate for ALL is now over 90%. However, some children with certain genetic profiles still have a much lower chance of survival, sometimes less than 40%.
Dr Laurence Cheung is dedicated to finding better treatments for these high-risk patients. His research focuses on how leukaemia develops in the bone marrow and how cancer cells interact with their surroundings, known as the leukaemia microenvironment. He is particularly interested in whether improving the health of the microenvironment can lead to better outcomes for children with leukaemia.
While scientists have long studied the role of the microenvironment in solid tumours, they are just beginning to understand its importance in blood cancers. Little is known about how normal bone and bone marrow cells contribute to the start, progression, and relapse of leukaemia.
Dr Cheung's research targets the cells surrounding the leukaemia cells to reduce the impact of cancer and lessen the side effects of traditional treatments for all children diagnosed with ALL. He believes that attacking both the cancer cells and their surroundings could be a powerful way to treat patients.
“Every parent’s wish is to be able to spend quality time with their kids and watch them grow. It’s incredibly important to me that families whose children are diagnosed with cancer don’t have those opportunities taken away. That’s what keeps me motivated to find a cure."
- Dr Laurence Cheung
Laurence and his colleagues in Australia and the US have developed a model that mimics the bone loss seen in children with ALL at diagnosis. This model helps researchers understand how cells in the bone marrow communicate when leukaemia develops.
Recently, the team completed a study showing that targeting the leukaemia microenvironment can not only stop bone loss but also slow the progression of the disease. This is an incredibly exciting finding that could lead to new treatments for children with ALL.
Dr Mark Pinese – Genomic Childhood Cancer Risk Researcher
Project: Personalised Medicine
Childhood Cancer Institute, University of NSW

Cure Cancer alumni Dr Mark Pinese joined the newly formed Genomic Childhood Cancer Risk Group in January 2022, which aims to develop an understanding of why some children get cancer, and if childhood cancer can be predicted.
Although cancer is often thought of as a disease of the ageing, we know that even very young children can get cancer. Mark and his team are dedicated to understanding why this happens.
“If we can understand why a child gets cancer, we might be able to identify children at risk, so we can detect it early and treat it early to get the best results. Perhaps we can even prevent it from developing in the first place."
- Dr Mark Pinese
Mark recently set up a large study that aims to examine the genome of every child with cancer in NSW, as well as the genomes of their parents, to investigate the genetic basis of childhood cancer. Through generating reports for participating families about their risk of childhood cancer, Mark hopes to help them understand why their child has developed cancer, and potentially how to prevent it in the future.